What may sound like snoring could be a more severe condition known as obstructive sleep apnea (OSA). According to the American Academy of Sleep Medicine, 1% to 3% of children are affected by sleep apnea, which causes increased carbon dioxide levels, decreased development and sleep abnormalities.
Medical professionals diagnose OSA through a polysomnogram, or sleep study, which monitors sleep stages and records breathing rate, airflow, oxygen levels and heart rate. This is done through sensors placed on the scalp, temples, chest and legs and connected with wires.
The setup time for sleep studies, required for diagnosing sleep apnea, is time-consuming. Additionally, the large array of wires for each electrode is uncomfortable for sleeping children.
A team of former students in the Department of Biomedical Engineering at Texas A&M University worked on a new custom-designed cap for their capstone project that could be more effective in sleep studies and more conducive for diagnosing children with sleep apnea.
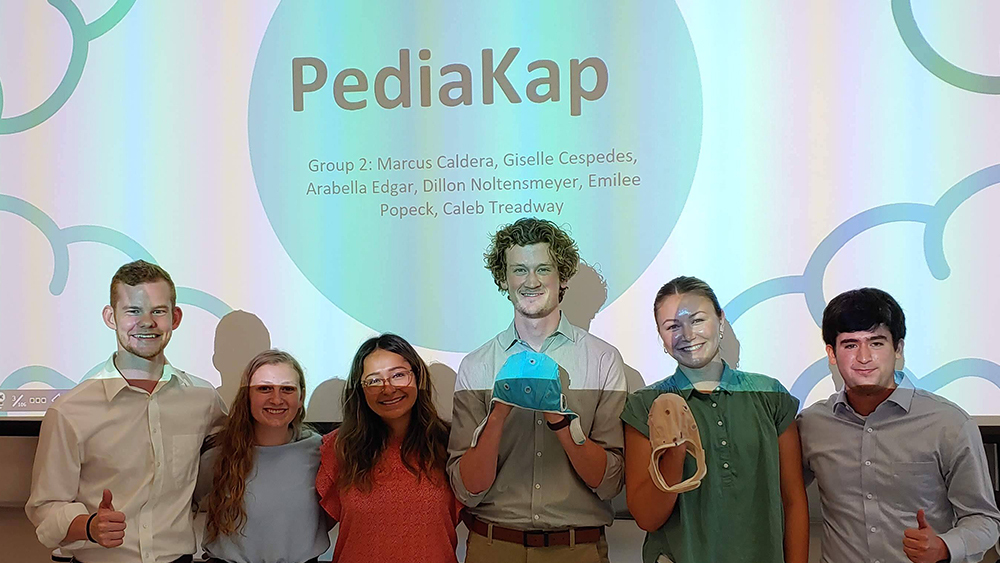
"Our device is essentially a custom-designed cap with 3D-printed electrode housing units placed in strategic positions around the head," said team member Dillon Noltensmeyer. "Our team proposed this solution after a series of brainstorming and redesigning sessions, which ultimately concluded in our final design."
The team used well-established polysomnogram protocols for electrode placement. Dr. Charles Peak, instructional assistant professor in the biomedical engineering department, said that when developing the design, the team thought about the ease of use and what would be comfortable for a child to wear during a sleep study.
The cap has sensors to monitor brain activity that allow for the incorporation of muscle tone sensors, a respiration monitor and heart rate measurements.
"This cap makes it more comfortable for the pediatric patient. It keeps all the wires together and just has a central cord that goes off more from the top of the head versus all these individual wires," Peak said.
According to Noltensmeyer, due to the time-consuming procedure at sleep study labs, there is a decrease in the number of patients that a particular sleep center can host, which has led to a backlog of patients not receiving treatment.
"If our solution was implemented nationwide, sleep studies could support a much larger volume of patients," he said.
This capstone project was sponsored and suggested by Dr. Kevin Kaplan from Texas Children's Hospital in Houston.
In addition to Noltensmeyer, team members included Marcus Caldera, Giselle Cespedes, Arabella Edgar, Emilee Popeck and Caleb Treadway. The team received the project in June 2021 and finished it shortly before graduating in May 2022.
Some students from the capstone project have entered professional engineering positions, while others have continued their education by pursuing master’s or doctoral degrees.
Peak said that overall, the ability to have connected with a doctor for the project helped the students and was a crucial part of their own development.