According to the American Heart Association, valvular heart disease affects about 2.5% of adults in the United States, and more than 100,000 patients undergo valve replacement surgery each year. Typically, replacement heart valves require a compromise between long-term durability and lowered risk of blood clots, causing patients to potentially need a subsequent surgery.
Researchers from Texas A&M University, with funding from Swiss heart valve company Novostia SA, are working to improve replacement heart valves so patients don’t have to compromise.
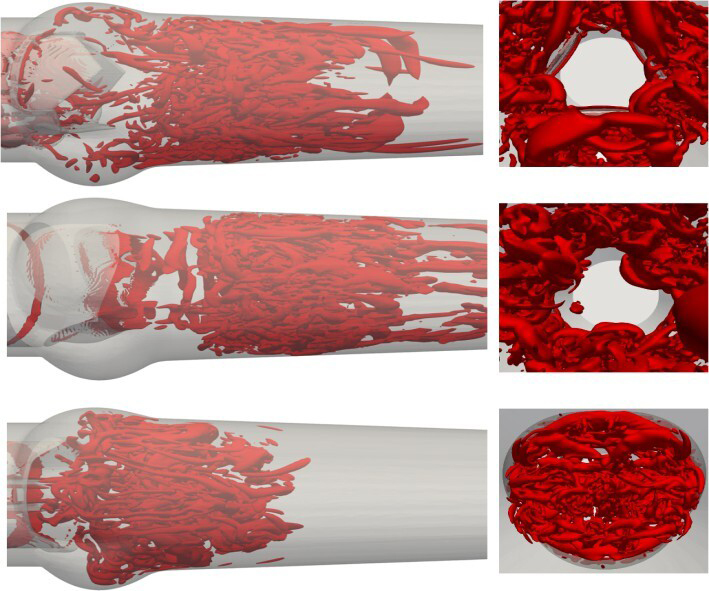
Mechanical heart valves typically feature two rigid leaflets that rotate in response to blood flow. Novostia is developing a trileaflet mechanical heart valve to mimic natural blood flow. Bioprosthetic valves, made from bovine or porcine tissue, have flexible leaflets that deform and rotate. These structural differences affect key factors of clotting risk including blood flow and valve closure mechanics.
Led by Dr. Iman Borazjani, a professor in the J. Mike Walker ’66 Department of Mechanical Engineering, the research team compared three replacement heart valve options — Novostia’s trileaflet mechanical valve, a bileaflet mechanical valve and a bioprosthetic valve that mimics the natural aortic valve — to study their impacts on blood flow mechanics.
“Our main goal was to compare the flow and valve kinematics of the trileaflet valve against the other two valves,” Borazjani said. “We found that the trileaflet valve begins to close during forward flow — similar to bioprosthetic valves — while the bileaflet valve only starts to close once backward flow begins. This distinction is critical because the primary function of a heart valve is to enforce unidirectional flow and minimize regurgitation.”
The study identified two fluid-dynamic principles that promote timely valve closure: a strong central jet, the deceleration of which reduces pressure in the central region, rather than the sinus area of the heart during late systole, and leaflet closure directed toward the center of the valvular opening. A better understanding of these principles allows researchers to improve the design of mechanical heart valves and reduce their regurgitant flow.
“For decades, mechanical heart valves have been constrained by a tradeoff between durability and clotting risk,” said Syed Samar Abbas, a mechanical engineering Ph.D. candidate who conducted simulations and analysis for the study. “By revealing the fluid-dynamic principles that govern valve closure, and understanding the main mechanism behind their clotting potential, our work moves us closer to overcoming this limitation.”
Researchers used a fluid-structure interaction framework to simulate valve behavior. Data analysis included examination of leaflet motion, pressure fields and flow velocities.
“We found that the trileaflet mechanical valve closes in a manner similar to the bioprosthetic valve across all simulations,” said Borazjani. “Our preliminary findings also showed reduced platelet activation, suggesting the potential for a valve that is both durable and biocompatible.”
Borazjani and Abbas are now developing a numerical framework to simulate platelet activation and clot formation in replacement heart valves. The first-of-its-kind model will account for both mechanical and biochemical stimuli acting on blood constituents under valve flow conditions.
“The design of prosthetic heart valves has not changed for decades,” Borazjani said. “With the new analysis tools, novel materials and manufacturing technologies of today, it is time for a new generation of heart valves to overcome the compromise between durability and clotting risks of artificial heart valves.”
Dr. Borazjani’s former Ph.D. student Hossein Asadi was also a collaborator on this project, working to develop the computational code used to simulate bioprosthetic valves.
This interdisciplinary project includes research techniques from computer science, bioengineering and clinical testing. With support from Novostia, the future of heart valve technology may be closer than ever to a safer, longer-lasting solution.